Friday, August 10th, 2012
Take the Plunge: Train for a Swim Race
Get your feet wet with one of these comprehensive swimming training plans
Read more at Women's Health: http://www.womenshealthmag.com/fitness/swim-training-plan#ixzz237d0ZWBxFriday, July 13th, 2012
Brain-eating amoebas blamed in three deaths
(CNN) -- It's eerie but it's true: Three people have died this summer after suffering rare infections from a waterborne amoeba that destroys the brain.This is the time of year when there is an uptick in cases. The amoebas flourish in the heat -- especially during the summer months in the South, thriving in warm waters where people swim.
Health officials usually record about two to three cases in a given year -- 1980 was the highest with eight deaths. And most of the time, they occur in children and teenagers.
"These are rare infections, but super tragic for families," said Jonathan Yoder, the waterborne disease and outbreak surveillance coordinator at the Centers for Disease Control and Prevention. "We don't want to minimize how hard it is for families."
 'Amoebas act extremely quickly'
'Amoebas act extremely quickly'
A 16-year-old died Saturday after becoming infected by an amoeba in Brevard County, Florida, according to CNN's affiliate WFTV. The amoeba could have entered the teen's body as the teen swam in a nearby river.
Her mother, P.J. Nash-Ryder, said her daughter complained of a headache, threw up 20 times and ran a fever as high as 104 degrees.
"She would sit up in bed and just look at me, and I would ask her what was wrong," Nash-Ryder said. "She would say, 'I don't know.' And I'd tell her to lay back down. Her eyes were rolling ... and she wouldn't shut them all the way."
A spinal tap showed that Naegleria fowleri was present in her spinal fluids.
In another case, the Virginia Department of Health confirmed Friday that a child from central Virginia died from primary amoebic meningoencephalitis, which is caused by the amoeba. The Richmond Times Dispatch said the child was a 9-year-old boy from Henrico County.
The child died within the last few weeks, said Dr. Keri Hall, the state's director of epidemiology. She declined to share other details. Virginia's last confirmed case was in 1969.
Amoeba infections in humans are extremely rare. The CDC found 32 reported cases in 10 years -- compared with 36,000 drowning deaths from 1996 to 2005.
Rare but deadly amoeba infection hard to prevent
The median age of the victims is 12, possibly because children and teenagers are more likely to play and swim in water. Nearly two-thirds of those killed by the amoeba are children under the age of 13.
The amoebas enter the human body through the nose after an individual swims or dives into warm fresh water, like ponds, lakes, rivers and even hot springs.
Lurking in fresh waters during the summertime, they're more likely to infect humans in July, August and September.
It's unclear why out of the millions of people who swim in the same fresh waters, a small fraction of people are infected by the amoeba.
"It's difficult to know," Yoder said. "It's not a disease that's easy to study because the end result is so severe. It's difficult to study in the lab."
Scientists speculate that the lack of certain antibodies could be why some children get infected, while others who've swum in the same water don't, said Francine Cabral, professor of microbiology at Virginia Commonwealth University School of Medicine.
The amoeba is not a parasite. A human is an "accidental end point for the amoeba after it's forced up the nose," Yoder said. It does not seek human hosts.
But when an amoeba gets lodged into a person's nose, it starts looking for food. It ends up in the brain and starts eating neurons.
"It causes a great deal of trauma and a great deal of damage," Yoder said. "It's a tragic infection. It's right at the frontal lobe. It affects behavior and the core of who they are -- their emotions, their ability to reason -- it's very difficult."
Early symptoms include headache, fever, nausea, vomiting and neck stiffness. Later symptoms include confusion, lack of attention to people and surroundings, loss of balance, seizures and hallucinations.
The amoeba multiplies, and the body mounts a defense against the infection. This, combined with the rapidly increasing amoebas, cause the brain to swell, creating immense pressure. At some point, the brain stops working.
Death typically occurs three to seven days after the symptoms start.
At hospitals, the infection is often mistaken for bacterial meningitis. Even when the diagnosis is made, the infection is difficult to treat.
The primary treatment for Naegleria infection is amphotericin B, an antifungal medication injected into the veins and brain.
But so far, only one person -- back in 1978 -- is known to have survived an infection, Yoder said.
Everybody panics because the amoeba infection is so deadly, but Cabral reminded: "The incidence of this disease is very very small, but when it happens it's tragic."
Here are the CDC's tips for prevention:
* Refrain from activities in warm, untreated or poorly treated water, especially when water levels are low and temperatures are high.
* Hold the nose shut or use nose clips when swimming in warm fresh water.
* Avoid digging or stirring up underwater sediments while submerged in shallow, warm
freshwater areas.
The Parasite Picture Library
WARNING: This Page May Disturb You!!!
An extraordinary variety of viruses, bacteria, parasites, and organisms stand ready to attack us and feed
off our bodies' cells. Using microscopes of varying power, photographers
show us a teeming microbial world that we could barely imagine without their help.
The approximate sizes of microbes can be approximated by using the following rule of thumb:
- VIRUSES are the smallest of all infectious agents, averaging about 100 nanometers (100 billionths of a meter) in length. They have so few genes and proteins of their own that in order to reproduce they need to commandeer the machinery of the cells they invade.
- BACTERIA vary widely in size and shape, but tend to be at least 10 times larger than viruses, or at least 1 micrometer (1 millionth of a meter) long. They are single-cell organisms that reproduce independently.
- SINGLE-CELL ORGANISMS tend to be at least 10 times larger than bacteria, or about .01 millimeter long.
- MULTI CELLULAR ORGANISMS are so large they can usually be seen with the naked eye. Tapeworms, for instance, can reach a length of 6 meters (20 feet).

Food and water are the
most common sources of parasite and invading organism transmission.
Since most of us eat three times a day and drink water frequently
throughout the day,
our exposure to these sources is constant. Tap water has been found to
be contaminated with harmful organisms. Both plant and animal foods
carry parasites,
and cleaning and cooking methods often do not often destroy them before
ingestion. The CDC (Center for Disease Control) cites food as the
catalyst behind 80 percent
of the pathogenic outbreaks in the U.S. Most are linked to restaurants
and delis where less than sanitary conditions exist -- from food
preparation and storage
to the utensils and servers' hands.

Animals, just like humans, can become infected with parasites and unhealthy organisms. Internally, contaminated water and food can spread the problem to our pets. Externally, animals become infected by organisms on their bodies, especially on their fur, because of exposure to infected animal wastes. Forgetting to wash your hands even one time after handling or cleaning up after your animal can transmit the parasite to you. Pets are a wonderful part of our lives. They provide comfort, companionship, protection, amusement, and unconditional love for their owners. Yet, pets, like humans, are often victims of serious infections that can unintentionally be passed on to their owners. In fact, there is a whole set of diseases classified as 'zoonoses' (animal-transmitted diseases) in parasitology textbooks. Animals are major carriers of harmful organisms, and most physicians, let alone the general public, are seemingly unaware of this fact. Experts have projected that of the 110 million pet dogs and cats in this country, over half may be infected with at least one or more different kinds of harmful organisms. Considering these numbers, the potential for transmission of parasitical invading organism infection from animals to humans is extremely high. Making a parasite cleanse an essential part of an effective health maintenance program for both people and animals alike.

The CDC estimates that the number of parasites present in the United States alone number in the thousands. These harmful organisms are biochemically complex creatures in their life histories, development, reproductive cycles, nutritional requirements, and manifestation. They are categorized according to structure, shape, function, and reproductive ability. These include microscopic organisms (protozoa); roundworms, pinworms, whipworms, and hookworms (nematoda); tapeworms (cestoda); and flukes (trematoda).
PROTOZOA
 Making
up approximately 70 percent of all invading organisms, protozoa are
invisible to the naked eye. They are one-celled microscopic organisms,
but don't let their
size fool you. Certain protoans, through their intensely rapid
reproductive ability, can take over the intestinal tract of their host;
and from there go on
to other organs and tissues. Some feed on red blood cells. Some protozoa
produce cysts - closed sacs in which they may be safely transported
through food
and water from one person to another. In the cyst state, protozoans are
safe from destruction by human digestive juices. These one-celled
'vampires'
can actually destroy the tissues of their hosts. According to experts,
an estimated 7 million people across the U.S. have some form of protozoa
living inside of them.
Common protozoa include: Endolimax nana, Giardia lamblia, Entamoeba histolytica, Cryptosporidum parvum, Blastocystis hominis,
Trichomonas vaginalis, Toxoplasma gondii, Cyclospora cayetanensis, Cryptosporidium muris, Pneumocystis carinii,
Plasmodium malariae, Plasmodium ovale, Plasmodium vivax, Plasmodium falciparum, Leishmania donovani,
Leishmania tropica, and Leishmania braziliensis.
Making
up approximately 70 percent of all invading organisms, protozoa are
invisible to the naked eye. They are one-celled microscopic organisms,
but don't let their
size fool you. Certain protoans, through their intensely rapid
reproductive ability, can take over the intestinal tract of their host;
and from there go on
to other organs and tissues. Some feed on red blood cells. Some protozoa
produce cysts - closed sacs in which they may be safely transported
through food
and water from one person to another. In the cyst state, protozoans are
safe from destruction by human digestive juices. These one-celled
'vampires'
can actually destroy the tissues of their hosts. According to experts,
an estimated 7 million people across the U.S. have some form of protozoa
living inside of them.
Common protozoa include: Endolimax nana, Giardia lamblia, Entamoeba histolytica, Cryptosporidum parvum, Blastocystis hominis,
Trichomonas vaginalis, Toxoplasma gondii, Cyclospora cayetanensis, Cryptosporidium muris, Pneumocystis carinii,
Plasmodium malariae, Plasmodium ovale, Plasmodium vivax, Plasmodium falciparum, Leishmania donovani,
Leishmania tropica, and Leishmania braziliensis.NEMATODE
 While
the protozoans are only single-celled, nematode creatures are multi
cellular. The adult worms multiply by producing eggs called ova or
larvae. The eggs usually
become infectious in soil or in an intermediate host before humans are
infected. It is interesting to note that unless the worm infection is
heavy, many individuals
do not show signs of infestation. While it may be unpleasant to
consider, it is true that the human host can coexist quite comfortably
with a few worms, unless they
reproduce in great numbers and create organ obstruction. Experts claim
that 'some type of worm is
already in the intestines of over 75 percent of the world's population'.
This is a frightening statement.
Common nematode include: Roundworm (Ascaris lumbricoides), Hookworm (Necator Americanus, Ancylostoma duodenal), Pinworm (Enterobius vermicularis),
Roundworm (Toxocara canis, Toxocara cati), Heart worm (Dirofilaria immitis), Strongyloides (Stronglyoides stercoralis), Trichinella (Trichinella spiralis),
Filaria (Wuchereria bancrofti, Brugia malayi, Onchocerca volvulus,
Loa loa, Mansonella streptocerca, Mansonella perstans, Mansonella
ozzardi), and Anisakine larvae.
While
the protozoans are only single-celled, nematode creatures are multi
cellular. The adult worms multiply by producing eggs called ova or
larvae. The eggs usually
become infectious in soil or in an intermediate host before humans are
infected. It is interesting to note that unless the worm infection is
heavy, many individuals
do not show signs of infestation. While it may be unpleasant to
consider, it is true that the human host can coexist quite comfortably
with a few worms, unless they
reproduce in great numbers and create organ obstruction. Experts claim
that 'some type of worm is
already in the intestines of over 75 percent of the world's population'.
This is a frightening statement.
Common nematode include: Roundworm (Ascaris lumbricoides), Hookworm (Necator Americanus, Ancylostoma duodenal), Pinworm (Enterobius vermicularis),
Roundworm (Toxocara canis, Toxocara cati), Heart worm (Dirofilaria immitis), Strongyloides (Stronglyoides stercoralis), Trichinella (Trichinella spiralis),
Filaria (Wuchereria bancrofti, Brugia malayi, Onchocerca volvulus,
Loa loa, Mansonella streptocerca, Mansonella perstans, Mansonella
ozzardi), and Anisakine larvae.CESTODA
 Among
the oldest known parasites, tapeworms are considered humanity's largest
intestinal inhabitant. They each have a scolex (head) that attaches to
the intestinal wall.
As long as the head remains attached to the intestinal mucosa, a new
worm can grow from it. Tapeworms do not contain digestive tracts but get
their nourishment by
absorbing partially digested substances from the host. They are whitish
in color, flat, and ribbon-like, with a covering that is a transparent
skin-like layer.
Common cestoda include: Beef tapeworm (Taenia saginata), Pork tapeworm (Taenia solium), Fish tapeworm (Diphyllobothrium latum), and Dog tapeworm (Dipylidium caninum).
Among
the oldest known parasites, tapeworms are considered humanity's largest
intestinal inhabitant. They each have a scolex (head) that attaches to
the intestinal wall.
As long as the head remains attached to the intestinal mucosa, a new
worm can grow from it. Tapeworms do not contain digestive tracts but get
their nourishment by
absorbing partially digested substances from the host. They are whitish
in color, flat, and ribbon-like, with a covering that is a transparent
skin-like layer.
Common cestoda include: Beef tapeworm (Taenia saginata), Pork tapeworm (Taenia solium), Fish tapeworm (Diphyllobothrium latum), and Dog tapeworm (Dipylidium caninum).TREMATODE
 Trematode
are leaf-shaped flatworms also known as flukes. They are parasitic
during nearly all of their life-cycle forms. The cycle begins when
larvae are released into
freshwater by infected snails. The free-swimming larvae can then
directly penetrate the skin of the human host or are ingested after
encysting in or on various edible, vegetation, fish, or crustaceans.
Common trematode include: Intestinal fluke (Fasciolopsis buski), Blood fluke (Schistosoma japonicum, Schistosoma mansoni) Schistosoma haematobium), Liver fluke (Clonorchis sinensis),
Oriental lung fluke (Paragonimus westermani), and Sheep liver fluke (Fasciola hepatica).
Trematode
are leaf-shaped flatworms also known as flukes. They are parasitic
during nearly all of their life-cycle forms. The cycle begins when
larvae are released into
freshwater by infected snails. The free-swimming larvae can then
directly penetrate the skin of the human host or are ingested after
encysting in or on various edible, vegetation, fish, or crustaceans.
Common trematode include: Intestinal fluke (Fasciolopsis buski), Blood fluke (Schistosoma japonicum, Schistosoma mansoni) Schistosoma haematobium), Liver fluke (Clonorchis sinensis),
Oriental lung fluke (Paragonimus westermani), and Sheep liver fluke (Fasciola hepatica).


Roundworm Click here for more info. |

Pinworm / Threadworm Click here for more info. |

Hookworm Click here for more info. |

Dwarf Tape worm Click here for more info. |
Whipworm Click here for more info. |

Fish Tapeworm Click here for more info. |

Intestinal Fluke Click here for more info. |

Amoeba Organisms Click here for more info. |
| Internal Body Camera Footage of a Parasitic Infestation. |
| Colonoscopy video: A large worm makes its home deep inside of a human host. |
| VNN News: Our loving pets may be transmitters of parasitical organisms. |
| FOX News: A woman mis-diagnosed with a brain tumor in fact had worms in her brain. |
| A shocking video of parasitical worms living in a man's face. |
| Parasites infect a man's eyes through usage of a contact lens. |
Friday, July 13th, 2012
Toxocariasis (aka Roundworm Infection) - Parasites
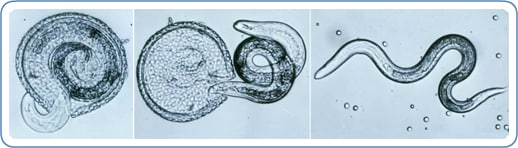
Toxocariasis is the parasitic disease caused by the larvae of two species of Toxocara roundworms: Toxocara canis from dogs and, less commonly, Toxocara cati from cats. Toxocariasis is considered one of the Neglected Parasitic Infections, a group of five parasitic diseases that have been targeted by CDC for public health action.
Image: Various stages of Toxocara canis larva hatching. Credit: DPDx
Disease
Most people infected with Toxocara do not have any
symptoms. There are two major forms of toxocariasis, visceral
toxocariasis, also called visceral-larva migrans (VLM) and ocular
toxocariasis, also called ocular larva migrans (OLM). The syndromes VLM
and OLM can be caused by infection with the migrating larvae of other
kinds of parasites which cause symptoms similar to those caused by
migrating Toxocara larvae.
In a few people who are infected with high numbers of Toxocara larvae or have repeated infections, the larvae can travel through parts of the body such as the liver, lungs, or central nervous system and cause symptoms such as fever, coughing, enlarged liver or pneumonia. This form of toxocariasis is called visceral toxocariasis or VLM. Rarely, the larvae can travel to the eye and cause ocular toxocariasis or OLM. Ocular toxocariasis occurs when a microscopic Toxocara larva enters the eye and causes inflammation and scarring on the retina. OLM can cause blindness.
In a few people who are infected with high numbers of Toxocara larvae or have repeated infections, the larvae can travel through parts of the body such as the liver, lungs, or central nervous system and cause symptoms such as fever, coughing, enlarged liver or pneumonia. This form of toxocariasis is called visceral toxocariasis or VLM. Rarely, the larvae can travel to the eye and cause ocular toxocariasis or OLM. Ocular toxocariasis occurs when a microscopic Toxocara larva enters the eye and causes inflammation and scarring on the retina. OLM can cause blindness.
Diagnosis
If you think you or your child may have toxocariasis, you should see
your health care provider to discuss the possibility of infection and,
if necessary, to be examined. Toxocariasis can be difficult to diagnose
because the symptoms of toxocariasis are similar to the symptoms of
other infections. A blood test is available that looks for evidence of
infection with Toxocara larvae. In addition to the blood test,
diagnosis of toxocariasis includes identifying the presence of typical
clinical signs of OLM or VLM and a history of exposure to cats and
dogs.
Read More Information
Treatment
Visceral toxocariasis can be treated with antiparasitic drugs such as albendazole or mebendazole, usually in combination with anti-inflammatory medications. Treatment of ocular toxocariasis is more difficult and usually consists of measures to prevent progressive damage to the eye.Prevention & Control
Controlling Toxocara infection in dogs and cats will reduce
the number of infectious eggs in the environment and reduce the risk
for people. Have your veterinarian treat your dogs and cats, especially
young animals, regularly for worms. This is especially important if
your pets spend time outdoors and may become infected again.
There are several things that you can do around your home to make you and your pets safer:
- Clean your pet’s living area at least once a week. Feces should be either buried or bagged and disposed of in the trash.
- Do not allow children to play in areas that are soiled with pet or other animal stool and cover sandboxes when not in use to make sure that animals do not get inside and contaminate them.
- Wash your hands with soap and warm water after playing with your pets or other animals, after outdoor activities, and before handling food.
- Teach children the importance of washing hands to prevent infection.
- Teach children that it is dangerous to eat dirt or soil.
More on: Handwashing
Toxocara eggs have a strong protective
layer which makes the eggs able to survive in the environment for
months or even years under the right conditions. Many common
disinfectants are not effective against Toxocara eggs but
extreme heat has been shown to kill the eggs. Prompt removal of animal
feces can help prevent infection since the eggs require a week or more
to become infective once they are out of the animal.
Read More Information


No comments:
Post a Comment